Understanding the GHS Index and Its Role in Global Health Analysis
Author:XTransfer2025.07.22GHS
The Global Health Security (GHS) Index evaluates health security across 195 countries, offering a benchmark to understand global preparedness for health threats. It highlights critical gaps in readiness, such as the fact that no country achieved a top-tier score in its 2021 assessment. You can see this reflected in the global average score of 38.9 out of 100, with prevention of pathogen emergence scoring even lower at 28.4. These figures reveal vulnerabilities that the COVID-19 pandemic further exposed, including insufficient health capacity in 70% of countries and a lack of emergency response plans in 176 nations. By using the GHS index, you gain insights into how health systems can better prepare for future pandemics and improve global health security.
What Is the Global Health Security Index?

Definition and Purpose
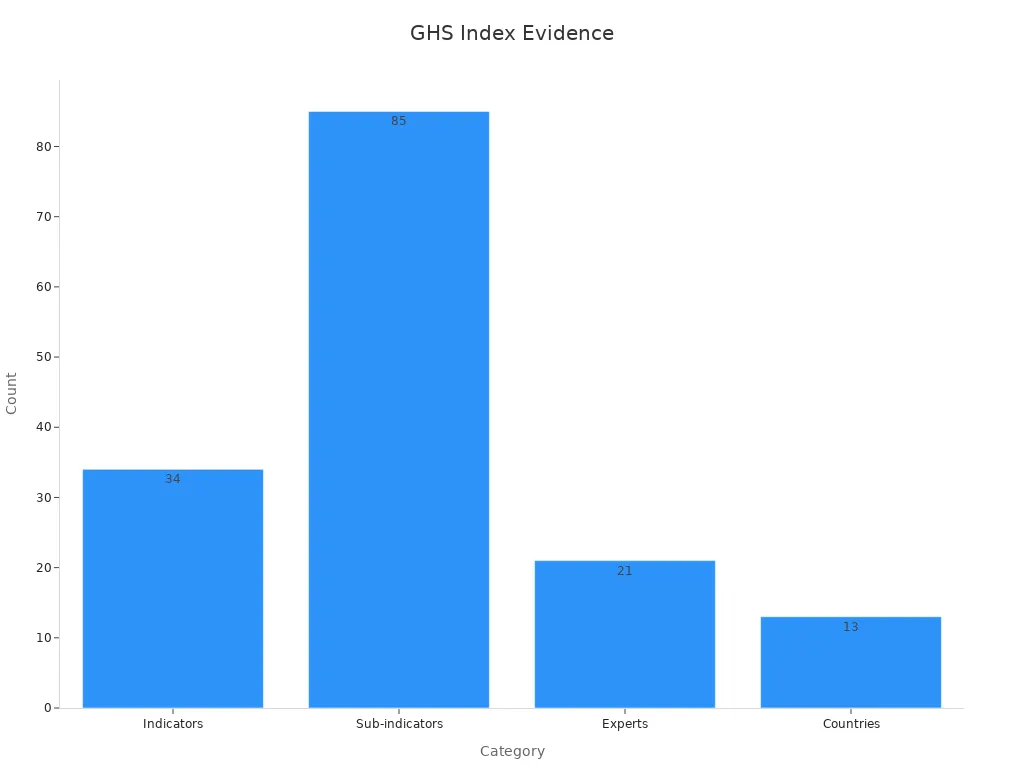
The Global Health Security Index serves as a comprehensive tool to evaluate how well countries can prevent, detect, and respond to health threats. It measures the level of preparedness across 195 nations, offering a clear picture of global health security. The index uses 34 indicators and 85 sub-indicators to assess various aspects of health systems, emergency response capabilities, and risk management. Each indicator is scored on a scale from 0 to 100, ensuring consistency in data comparison.
|
Indicator Count |
Description |
|
34 |
Total number of indicators in the GHS Index |
|
85 |
Total number of sub-indicators in the GHS Index |
|
0-100 |
Scoring scale used for normalizing data |
|
21 |
Number of experts in the GHS Index International Panel of Experts |
|
13 |
Number of countries represented in the expert panel |
The index helps you understand where countries stand in terms of pandemic preparedness and highlights areas needing improvement. By focusing on prevention, detection, and response, it provides a roadmap for strengthening health systems worldwide.
Development and Key Stakeholders
The Global Health Security Index was developed through a collaborative effort involving leading health organizations and experts. The Nuclear Threat Initiative (NTI) and the Johns Hopkins Center for Health Security spearheaded its creation, with support from the Economist Intelligence Unit. These organizations worked closely with an international panel of 21 experts from 13 countries, ensuring a diverse and well-rounded perspective.
The World Health Organization (WHO) and other global institutions also contributed valuable insights. Their involvement ensured that the index aligns with international health standards and priorities. This collaboration underscores the importance of collective action in addressing global health challenges.
Importance for Health Security
The Global Health Security Index plays a vital role in improving health security worldwide. It identifies gaps in preparedness, helping countries prioritize investments and policy changes. For example, the index revealed that most nations scored poorly in areas like pathogen prevention and emergency response. These findings highlight the urgent need for stronger health systems.
You can use the index to understand how well countries are equipped to handle pandemics like COVID-19. It also serves as a benchmark for tracking progress over time. By addressing weaknesses identified in the index, countries can enhance their level of preparedness and reduce the impact of future health crises.
The COVID-19 pandemic demonstrated the importance of global health security. Many countries struggled with inadequate resources and delayed responses, leading to poor COVID-19 outcomes. The index provides a framework for avoiding similar challenges in the future. It emphasizes the need for coordinated efforts and robust health systems to protect populations from emerging threats.
How Does the GHS Index Assess Health Security?
Framework Overview
The GHS Index evaluates health security by examining six critical aspects of preparedness. These include prevention, detection and reporting, rapid response, health systems, compliance with international norms, and risk environment. Each aspect focuses on a specific area of global health security. For example, prevention assesses measures to stop outbreaks before they occur, while detection and reporting evaluate systems for identifying and sharing information about health threats. Rapid response measures how quickly a country can act during emergencies. The framework also considers the strength of healthcare infrastructure and adherence to global health standards set by organizations like the World Health Organization. Finally, it examines factors that increase vulnerability to health threats, such as political instability or weak governance.
|
Aspect of Preparedness |
Description |
|
Prevention |
Measures taken to prevent outbreaks from occurring. |
|
Detection and Reporting |
Systems in place for identifying and reporting health threats. |
|
Rapid Response |
Ability to respond quickly to health emergencies. |
|
Health Systems |
Strength and resilience of the healthcare infrastructure. |
|
Compliance with International Norms |
Adherence to global health regulations and standards. |
|
Risk Environment |
Assessment of factors that may increase vulnerability to health threats. |
This structured framework ensures a comprehensive evaluation of a country's ability to handle health emergencies, including pandemics like COVID-19.
Categories and Indicators
The GHS Index uses six main categories to assess health security. These categories are divided into 34 indicators and 85 sub-indicators. Each indicator focuses on a specific element of preparedness, such as laboratory systems, emergency response plans, or healthcare access. By breaking down health security into these smaller components, the index provides a detailed picture of a country's strengths and weaknesses. For instance, countries with robust laboratory systems score higher in detection and reporting, while those with weak emergency plans may score lower in rapid response. This detailed approach helps you understand where improvements are needed to enhance global health security.
Scoring and Ranking Methodology
The GHS Index employs a detailed scoring system to rank countries based on their level of preparedness. It evaluates 140 specific questions across the six categories, assigning scores from 0 to 100 for each indicator. These scores are then averaged to calculate a country's overall ranking. This methodology ensures consistency and fairness in comparing health security capabilities. For example, a country with strong prevention measures but weak healthcare infrastructure may receive a moderate overall score. The index also highlights disparities in preparedness, such as the low global average score of 38.9 out of 100. By identifying these gaps, the GHS Index helps guide investments and policy changes to improve health security worldwide.
Key Findings of the GHS Index

Global Preparedness Gaps
The Global Health Security Index reveals significant gaps in global preparedness for health emergencies. Many countries struggle to meet the standards required to prevent, detect, and respond to pandemics effectively. For instance, fewer than 7% of countries rank in the highest tier for preventing the emergence or release of pathogens. Similarly, less than 5% demonstrate strong capabilities for rapid response and mitigation of disease spread. These statistics highlight the urgent need for improvement in health security systems worldwide.
|
Category |
Percentage of Countries in Highest Tier |
Average Score (out of 100) |
|
Prevention of the emergence or release of pathogens |
< 7% |
N/A |
|
Early detection and reporting of epidemics |
19% |
66.7 |
|
Rapid response to and mitigation of spread |
< 5% |
N/A |
|
Sufficient and robust health sector |
N/A |
26.4 |
The low average score of 26.4 for health sector robustness underscores the challenges many nations face in building resilient healthcare systems. These gaps became evident during the COVID-19 pandemic, where inadequate resources and delayed responses led to poor outcomes in many regions. Addressing these weaknesses is essential to improving the level of preparedness for future health crises.
Regional Strengths and Weaknesses
Preparedness levels vary significantly across regions. The Americas, Europe, and Southeast Asia generally perform better in health security compared to Africa. Socioeconomic factors and the strength of health systems play a crucial role in these differences. Wealthier regions often have more resources to invest in healthcare infrastructure and emergency response systems, while lower-income areas face greater challenges.
-
The Americas and Europe show higher levels of preparedness due to stronger health systems and better access to resources.
-
Southeast Asia demonstrates progress in areas like early detection and reporting, but gaps remain in rapid response capabilities.
-
Africa struggles with limited resources and weaker health systems, making it more vulnerable to pandemics.
From 2019 to 2021, a concerning trend emerged. Preparedness levels declined globally, emphasizing the need for renewed focus on strengthening health systems. The World Health Organization (WHO) has called for increased collaboration and investment to address these disparities and improve global health security.
Case Studies of Country Performance
Examining individual countries provides valuable insights into the strengths and weaknesses of health security systems. For example, the United States scored relatively high in early detection and reporting but faced challenges in rapid response during the COVID-19 pandemic. This highlights the importance of balancing strengths across all categories of the GHS.
In contrast, countries like Vietnam and South Korea demonstrated effective responses to COVID-19. Their success stemmed from robust prevention measures, efficient contact tracing, and strong public health campaigns. These examples show how targeted investments in specific areas can lead to better outcomes during health emergencies.
On the other hand, many low-income countries struggled to manage the pandemic due to limited resources and weak healthcare infrastructure. These challenges underscore the need for global cooperation and support to ensure all nations can improve their level of preparedness.
Practical Implications for Global Health Security
Policy Guidance and Investment Priorities
Strengthening global health security requires targeted investments and clear policy guidance. You can focus on areas like pathogen prevention, healthcare infrastructure, and emergency response systems to improve the level of preparedness. Cost-benefit analyses provide valuable insights into prioritizing these investments. For example, the Value of Statistical Life (VSL) highlights the importance of considering age and life expectancy when allocating resources. Younger populations often benefit more from health interventions due to their longer life expectancy. Similarly, the Cost of Illness (COI) framework measures direct costs and productivity losses but emphasizes the need to account for quality of life impacts. These tools help policymakers make informed decisions that maximize the benefits of health investments.
|
Aspect |
Description |
|
Value of Statistical Life |
Adjusts based on age and life expectancy, prioritizing younger populations. |
|
Cost of Illness |
Measures direct costs and productivity losses, focusing on quality of life. |
By using these frameworks, you can ensure that resources are allocated efficiently to address critical gaps in health security.
Collaboration in Global Health Strategies
Collaboration plays a vital role in addressing global health challenges. The COVID-19 pandemic underscored the importance of equitable research partnerships and cross-cultural cooperation. You can look to examples like the United Nations and the World Health Organization, which emphasize innovative research and capacity building in public health. These organizations have worked to generate knowledge tailored to the needs of low and middle-income countries (LMICs).
-
Equitable research partnerships during the COVID-19 pandemic highlighted the value of shared knowledge.
-
Cross-country collaboration has proven essential for addressing health disparities in LMICs.
-
Capacity-building initiatives by organizations like WHO have strengthened public health systems globally.
By fostering collaboration, you can help bridge gaps in national health security and improve outcomes during future pandemics.
Role of XTransfer in Supporting Stakeholders
XTransfer offers a unique solution for stakeholders aiming to enhance global health security. Its exchange rate platform simplifies international transactions, ensuring that funds reach their intended destinations efficiently. This capability is crucial for supporting health initiatives in resource-limited settings. For example, during the COVID-19 pandemic, timely funding played a critical role in vaccine distribution and emergency response efforts. By using XTransfer, you can streamline financial processes, enabling faster implementation of health programs and emergency plans. This tool empowers stakeholders to focus on improving health systems and addressing preparedness gaps without financial delays.
Using the GHS Index to Improve Health Security
The GHS Index remains a critical tool for evaluating and improving global health security. It helps you identify weaknesses in health systems and prioritize areas for improvement. The lessons from COVID-19 highlight the urgency of addressing these gaps. Coordinated global efforts can strengthen prevention, detection, and response capabilities. By leveraging tools like the GHS Index and XTransfer’s platform, you can ensure resources are allocated effectively. These steps will prepare health systems to face future challenges and protect populations worldwide.
FAQ
What is the purpose of the GHS Index?
The GHS Index helps you understand how prepared countries are to handle health emergencies. It identifies gaps in prevention, detection, and response systems, guiding improvements in global health security.
How often is the GHS Index updated?
The GHS Index is updated every two years. This schedule ensures you get the most accurate and relevant data to assess global health preparedness.
Why do some countries score lower on the GHS Index?
Countries may score lower due to weak healthcare systems, limited resources, or insufficient emergency plans. These factors reduce their ability to prevent, detect, and respond to health threats effectively.
Can the GHS Index predict future pandemics?
No, the GHS Index does not predict pandemics. Instead, it evaluates preparedness levels, helping you understand how well countries can manage potential health crises.
How can you use the GHS Index to improve health security?
You can use the GHS Index to identify weaknesses in health systems and prioritize investments. It provides a roadmap for strengthening prevention, detection, and response capabilities worldwide.
Related content